Unlocking the Secrets of PCOS: A Technological Transformation
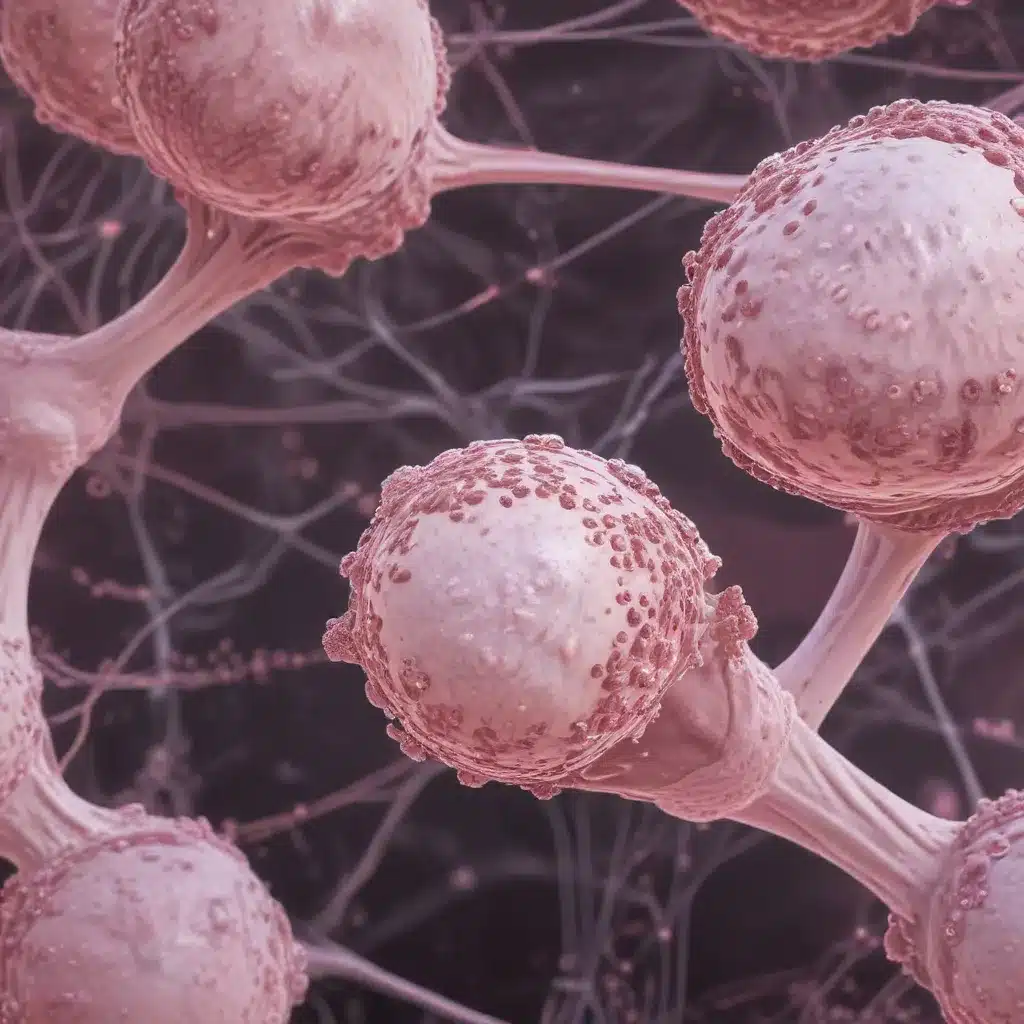
Polycystic Ovary Syndrome (PCOS) has long been a complex and challenging condition affecting millions of women globally. This endocrine disorder, characterized by hormonal imbalances, ovarian abnormalities, and a wide range of symptoms, has traditionally posed significant diagnostic and treatment hurdles. However, the rapid advancements in artificial intelligence (AI) and machine learning (ML) have revolutionized the way we approach PCOS, offering new hope for early detection, personalized management, and improved patient outcomes.
The traditional approach to PCOS diagnosis has been fraught with challenges. Clinicians often rely on a combination of clinical assessments, biochemical tests, and imaging techniques, such as ovarian ultrasounds, to identify the condition. This multi-faceted approach can be time-consuming, expensive, and subject to variations in interpretation, leading to delayed or inaccurate diagnoses. Furthermore, the heterogeneous nature of PCOS, with its diverse symptom presentations, has further complicated the diagnostic process, leaving many women undiagnosed or misdiagnosed.
The integration of AI and ML into the healthcare landscape has revolutionized the landscape of PCOS detection and management. These powerful technologies have the ability to analyze vast amounts of clinical data, including hormone levels, imaging scans, and patient histories, to identify patterns and correlations that are often overlooked by human clinicians. By leveraging machine learning algorithms, healthcare providers can now achieve more accurate and efficient PCOS diagnoses, leading to earlier interventions and better long-term outcomes for patients.
One of the key advancements in this field is the development of deep learning models, specifically convolutional neural networks (CNNs), for the analysis of PCOS-related ultrasound images. These AI-powered systems can automatically identify and quantify ovarian abnormalities, such as the presence and size of follicles, with a level of precision and consistency that surpasses manual assessment. By integrating these deep learning models into the diagnostic workflow, clinicians can streamline the process, reduce the risk of human error, and provide more reliable diagnoses to their patients.
Moreover, the integration of wearable health devices and the Internet of Medical Things (IoMT) has further enhanced the potential for early PCOS detection and personalized management. These technologies allow for continuous monitoring of physiological parameters, such as blood sugar levels, heart rate, and physical activity, which are crucial indicators of the metabolic and cardiovascular complications associated with PCOS. By leveraging the data collected from these devices, healthcare providers can identify early warning signs, implement tailored interventions, and closely monitor the progression of the condition, ultimately improving patient outcomes.
Advancements in telemedicine and cloud-based healthcare platforms have also played a significant role in democratizing access to PCOS diagnosis and management. With the help of high-speed 5G technology, healthcare professionals can now remotely analyze medical images, review patient data, and provide personalized guidance to women, even in remote or underserved areas. This accessibility is particularly crucial for PCOS, as it enables early intervention and consistent monitoring, which are essential for managing the long-term risks associated with the condition.
In the realm of PCOS research and treatment, the integration of AI and ML has also led to the development of more personalized and targeted therapies. By analyzing large datasets of patient information, researchers can identify specific genetic and environmental factors that contribute to the development and progression of PCOS. This knowledge can then be used to design tailored interventions, such as lifestyle modifications, pharmacological treatments, or even precision-based therapies, that are optimized for individual patient needs.
As we delve deeper into the transformative power of AI and ML in PCOS management, it is clear that these technologies have the potential to revolutionize the way we approach this complex condition. By enabling earlier detection, personalized treatment, and more efficient healthcare delivery, these advancements hold the promise of improving the lives of millions of women affected by PCOS.
Harnessing the Power of AI and ML for PCOS Diagnosis
The traditional approach to Polycystic Ovary Syndrome (PCOS) diagnosis has long been a complex and time-consuming process, often involving a combination of clinical assessments, biochemical tests, and imaging techniques. However, the integration of artificial intelligence (AI) and machine learning (ML) into the healthcare landscape has revolutionized the way we approach PCOS detection and management.
One of the key breakthroughs in this field is the use of convolutional neural networks (CNNs), a type of deep learning architecture, in the analysis of PCOS-related ultrasound images. These AI-powered systems have demonstrated remarkable accuracy in identifying and quantifying ovarian abnormalities, such as the presence and size of follicles, with a level of precision that surpasses manual assessment by clinicians.
By leveraging the power of deep learning, these models can automatically extract and analyze intricate patterns within the ultrasound images, identifying subtle nuances that may be overlooked by human clinicians. This not only streamlines the diagnostic process but also reduces the risk of human error, leading to more reliable and consistent PCOS diagnoses.
Moreover, the integration of wearable health devices and the Internet of Medical Things (IoMT) has further enhanced the potential for early PCOS detection and personalized management. These technologies allow for continuous monitoring of physiological parameters, such as blood sugar levels, heart rate, and physical activity, which are crucial indicators of the metabolic and cardiovascular complications associated with PCOS.
By analyzing the data collected from these devices, healthcare providers can identify early warning signs, implement tailored interventions, and closely monitor the progression of the condition, ultimately improving patient outcomes. This personalized approach to PCOS management is a significant departure from the one-size-fits-all strategies of the past, paving the way for more effective and targeted care.
The advancements in telemedicine and cloud-based healthcare platforms have also played a crucial role in democratizing access to PCOS diagnosis and management. With the help of high-speed 5G technology, healthcare professionals can now remotely analyze medical images, review patient data, and provide personalized guidance to women, even in remote or underserved areas. This accessibility is particularly crucial for PCOS, as it enables early intervention and consistent monitoring, which are essential for managing the long-term risks associated with the condition.
In the realm of PCOS research and treatment, the integration of AI and ML has also led to the development of more personalized and targeted therapies. By analyzing large datasets of patient information, researchers can identify specific genetic and environmental factors that contribute to the development and progression of PCOS. This knowledge can then be used to design tailored interventions, such as lifestyle modifications, pharmacological treatments, or even precision-based therapies, that are optimized for individual patient needs.
As we continue to explore the transformative potential of AI and ML in PCOS management, it is clear that these technologies hold the key to unlocking more accurate, efficient, and personalized healthcare solutions for women affected by this complex condition. By enabling earlier detection, targeted interventions, and more streamlined healthcare delivery, these advancements have the power to dramatically improve the lives of millions of women worldwide.
Harnessing the Power of Machine Learning for Accurate PCOS Diagnosis
The traditional approach to diagnosing Polycystic Ovary Syndrome (PCOS) has long been a complex and challenging process, often requiring a combination of clinical assessments, biochemical tests, and imaging techniques. However, the rapid advancements in artificial intelligence (AI) and machine learning (ML) have transformed the landscape of PCOS detection and management, offering new hope for early and accurate diagnosis.
One of the key breakthroughs in this field is the use of machine learning algorithms to analyze clinical data and ultrasound images. By leveraging the power of these technologies, healthcare providers can now achieve more precise and consistent PCOS diagnoses, leading to earlier interventions and better long-term outcomes for patients.
Analyzing Clinical Data with Machine Learning
When it comes to PCOS diagnosis, clinical data plays a crucial role. Factors such as hormone levels, body mass index (BMI), and menstrual history can provide valuable insights into the underlying condition. Machine learning models, such as Logistic Regression (LR), Support Vector Machines (SVM), and Naive Bayes (NB), have demonstrated their ability to effectively analyze these complex datasets and identify patterns that may be missed by human clinicians.
In a recent study, researchers utilized a correlation-based feature extraction method to identify the most relevant clinical features for PCOS prediction. By applying this technique to a dataset of 541 PCOS cases, they were able to narrow down the number of features from 45 to 17, significantly reducing the complexity of the dataset while preserving the most important information.
When these extracted features were fed into various machine learning models, the results were impressive. The SVM model, in particular, achieved an accuracy of 94.44%, outperforming both Logistic Regression and Naive Bayes. This high level of accuracy can be attributed to SVM’s ability to effectively handle the nonlinear relationships and interdependencies inherent in PCOS-related clinical data.
Unlocking the Secrets of PCOS Ultrasound Imaging
In addition to clinical data, ultrasound imaging plays a crucial role in PCOS diagnosis. Traditionally, clinicians have relied on manual counting and measurement of ovarian follicles to identify the presence of polycystic ovaries. However, this process can be time-consuming, subjective, and prone to inconsistencies.
The integration of deep learning models, specifically convolutional neural networks (CNNs), has revolutionized the analysis of PCOS-related ultrasound images. These AI-powered systems can automatically detect and quantify ovarian abnormalities, such as the number and size of follicles, with a level of precision that surpasses human capabilities.
Moreover, the use of transfer learning, a technique where a pre-trained model (such as VGG16) is fine-tuned on the PCOS ultrasound dataset, has further enhanced the performance of these deep learning models. The VGG16 transfer learning approach has achieved an impressive validation accuracy of 98.29%, demonstrating its ability to effectively identify PCOS-related patterns in the ultrasound images.
Combining Clinical Data and Imaging for Optimal PCOS Diagnosis
While machine learning models have shown remarkable performance in analyzing either clinical data or ultrasound images individually, the true power of these technologies lies in their ability to integrate and leverage both data sources simultaneously.
By combining the insights gained from clinical features and ultrasound imaging, healthcare providers can achieve a more comprehensive and accurate PCOS diagnosis. This multifaceted approach not only enhances the overall diagnostic accuracy but also reduces the risk of missed or delayed diagnoses, which can have significant implications for patient outcomes.
Empowering Healthcare Providers with AI-Driven PCOS Solutions
The integration of AI and ML into the PCOS diagnostic process has the potential to transform the way healthcare providers approach this complex condition. By automating the analysis of clinical data and ultrasound images, these technologies can save time, reduce the burden on clinicians, and ensure more consistent and reliable diagnoses.
Moreover, the development of user-friendly, AI-powered PCOS diagnostic tools can empower healthcare providers, even those without specialized expertise in the field, to make more informed decisions and provide better care for their patients. This democratization of PCOS diagnosis can have far-reaching implications, particularly in underserved or remote regions where access to specialized care may be limited.
As we continue to explore the boundless potential of AI and ML in the realm of PCOS management, it is clear that these technologies hold the key to unlocking a future of more accurate, efficient, and personalized healthcare solutions for women affected by this condition. By harnessing the power of data-driven insights and cutting-edge algorithms, we can pave the way for earlier interventions, targeted therapies, and improved long-term outcomes for individuals living with PCOS.
Optimizing PCOS Prognosis through Deep Learning and Transfer Learning
Polycystic Ovary Syndrome (PCOS) is a complex endocrine disorder that affects millions of women worldwide, posing significant challenges in terms of diagnosis and management. Traditional approaches to PCOS detection have relied on a combination of clinical assessments, biochemical tests, and imaging techniques, such as ovarian ultrasounds. However, the heterogeneous nature of PCOS, with its diverse symptom presentations, has often led to delayed or inaccurate diagnoses, hindering early intervention and personalized treatment.
The advent of artificial intelligence (AI) and machine learning (ML) has revolutionized the landscape of PCOS detection and management, offering new hope for optimized prognosis and improved patient outcomes. One of the key advancements in this field is the integration of deep learning, a subset of machine learning, and transfer learning techniques to analyze PCOS-related ultrasound images.
Convolutional Neural Networks for PCOS Ultrasound Analysis
Convolutional Neural Networks (CNNs) have emerged as a powerful tool in the realm of medical image analysis, and their application to PCOS ultrasound imaging has been particularly impactful. These deep learning models are designed to automatically extract and learn features from the input images, identifying complex patterns and correlations that may be challenging for human clinicians to discern.
In the context of PCOS, CNNs can be trained to recognize the characteristic ovarian abnormalities, such as the presence and size of follicles, with a high degree of accuracy. By analyzing the ultrasound images, these AI-powered systems can provide clinicians with a comprehensive and quantitative assessment of the patient’s ovarian status, streamlining the diagnostic process and reducing the risk of subjective interpretation.
Harnessing the Power of Transfer Learning
While deep learning models like CNNs have demonstrated impressive performance in PCOS ultrasound analysis, the development of these models from scratch can be a time-consuming and resource-intensive process, particularly when working with limited training data.
This is where transfer learning comes into play. Transfer learning is a technique that leverages the knowledge gained from a pre-trained model, such as the well-known VGG16 architecture, and applies it to a new task or dataset. By fine-tuning the pre-trained model on the PCOS ultrasound dataset, researchers have been able to achieve remarkable results, with the VGG16 transfer learning approach outperforming the standalone CNN model with a validation accuracy of 98.29%.
The power of transfer learning lies in its ability to efficiently utilize the extensive knowledge and feature representations learned by the pre-trained model, which has been trained on a vast and diverse dataset. This approach allows the PCOS-specific model to build upon this foundational understanding, rather than starting from scratch, leading to faster convergence, better generalization, and higher overall performance.
Integrating Clinical Data and Imaging for Comprehensive PCOS Assessment
While the analysis of PCOS-related ultrasound images using deep learning and transfer learning has demonstrated impressive results, the true power of these technologies lies in their ability to integrate and leverage both clinical data and imaging information for a more comprehensive PCOS assessment.
By combining insights from clinical features, such as hormone levels, BMI, and menstrual history, with the quantitative analysis of ovarian abnormalities from ultrasound imaging, healthcare providers can achieve a more accurate and personalized PCOS diagnosis. This multifaceted approach not only enhances the overall diagnostic accuracy but also enables the development of tailored treatment plans, addressing the unique needs and characteristics of each individual patient.
Empowering Healthcare Providers with AI-Driven PCOS Solutions
The integration of deep learning and transfer learning into the PCOS diagnostic process has the potential to transform the way healthcare providers approach this complex condition. By automating the analysis of ultrasound images and leveraging the power of clinical data, these AI-driven solutions can save time, reduce the burden on clinicians, and ensure more consistent and reliable diagnoses.
Moreover, the development of user-friendly, AI-powered PCOS diagnostic tools can empower healthcare providers, even those without specialized expertise in the field, to make more informed decisions and provide better care for their patients. This democratization of PCOS diagnosis can have far-reaching implications, particularly in underserved or remote regions where access to specialized care may be limited.
As we continue to explore the boundless potential of deep learning and transfer learning in the realm of PCOS management, it is clear that these technologies hold the key to unlocking a future of more accurate, efficient, and personalized healthcare solutions for women affected by this condition. By harnessing the power of data-driven insights and cutting-edge algorithms, we can pave the way for earlier interventions, targeted therapies, and improved long-term outcomes for individuals living with PCOS.
Revolutionizing PCOS Diagnosis with AI-Powered Ultrasound Analysis
Polycystic Ovary Syndrome (PCOS) is a complex endocrine disorder that affects millions of women worldwide, characterized by a wide range of symptoms, including irregular menstrual cycles, excess androgen production, and ovarian abnormalities. Traditionally, the diagnosis of PCOS has relied on a combination of clinical assessments, biochemical tests, and imaging techniques, such as ovarian ultrasounds. However, this multifaceted approach can be time-consuming, subjective, and prone to inconsistencies, leading to delayed or inaccurate diagnoses.
The rapid advancements in artificial intelligence (AI) and machine learning (ML) have revolutionized the way healthcare providers approach PCOS detection and management. One of the most significant breakthroughs in this field is the integration of deep learning, a powerful subset












