Exploring the Effects on the Common Femoral Artery
As a seasoned IT professional, I’m excited to delve into the world of percutaneous endovascular aneurysm repair (PEVAR) and its impact on the common femoral artery (CFA). This cutting-edge surgical technique has revolutionized the treatment of abdominal aortic aneurysms, offering a minimally invasive alternative to traditional open surgery.
However, the current literature on the anatomical changes in the CFA post-PEVAR has been somewhat contradictory, with limited studies controlling for the potential confounding effects of ethnicity. This prompted me to investigate the topic further, drawing insights from recent research to provide practical guidance for IT Fix readers.
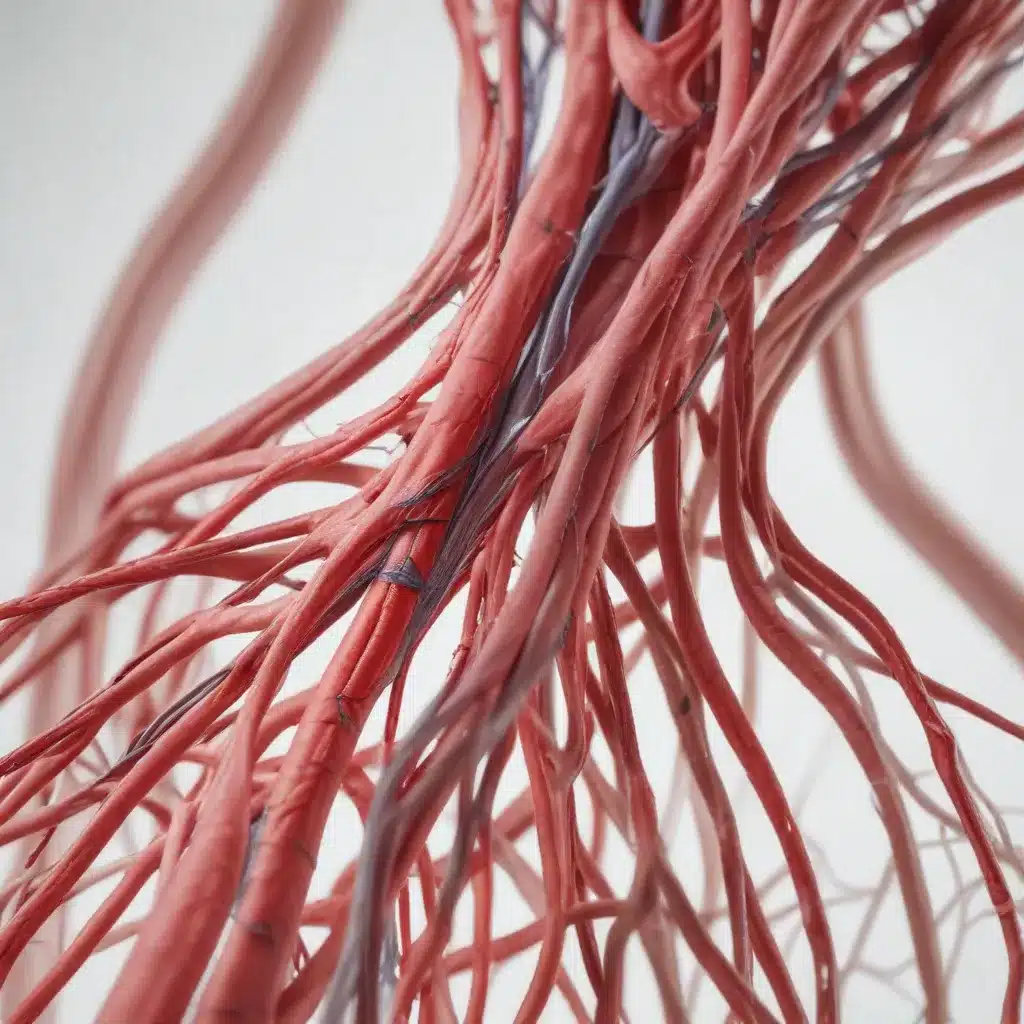
Understanding the Anatomy of the CFA
The CFA serves as the primary access site for PEVAR procedures, making it a crucial area of focus. Existing studies have explored the impact of PEVAR on the CFA’s inner luminal diameter (ID) and outer diameter (OD), the latter encompassing the arterial walls.
While some researchers have reported no significant changes in CFA dimensions after PEVAR, others have found statistically significant decreases in both the ID and OD. This discrepancy underscores the need for a more comprehensive understanding of the anatomical effects, particularly in diverse patient populations.
Investigating an Asian Study Cohort
To address this gap, a recent study published in CVIR Endovascular examined the anatomical changes in the CFA of an Asian patient cohort who underwent PEVAR. The researchers reviewed the records of 113 patients who received PEVAR at a Singapore hospital between January 2019 and September 2023.
By analyzing the pre- and post-operative computed tomography (CT) angiography scans of 117 groins, the study revealed some intriguing findings:
- The CFA ID exhibited a statistically significant decrease of 0.167 mm (p-value = 0.0403) after PEVAR.
- The CFA OD also decreased by a statistically significant 0.247 mm (p-value = 0.0107).
Importantly, these changes were observed regardless of the presence of common cardiovascular risk factors, such as diabetes mellitus, hypertension, and hyperlipidemia.
Implications for Patient Safety
While the observed decreases in CFA diameters were statistically significant, the researchers noted that the percentage changes were below the established flow-limiting values. This was reflected in the study’s findings, which reported only a single access site complication (a pseudoaneurysm) within the 3-month post-PEVAR period.
These results provide reassurance regarding the safety profile of PEVAR, even in an Asian population with a smaller baseline CFA lumen size. The authors suggest that the minimally invasive nature of PEVAR, coupled with the ability of the arterial walls to recover from the localized trauma, may contribute to the overall safety of the procedure.
Considering Longer-Term Effects
However, the researchers acknowledged the need for longer-term studies to fully characterize any late postoperative effects on the CFA. As with any surgical intervention, it’s crucial to monitor patients closely and assess the long-term implications of PEVAR on the structural integrity and functionality of the CFA.
By conducting similar studies with extended follow-up periods, the IT Fix community can gain a more comprehensive understanding of the long-term anatomical changes and their potential impact on patient outcomes. This knowledge will be invaluable in guiding clinicians and IT professionals alike in providing the most effective and safe care for individuals undergoing PEVAR.
Optimizing Percutaneous Endovascular Aneurysm Repair
As an IT professional, I’m always on the lookout for practical solutions that can improve patient outcomes and enhance the overall efficiency of healthcare systems. The growing adoption of PEVAR is a testament to the continued advancements in endovascular technology, and understanding the nuances of this procedure is crucial for IT professionals working in the medical field.
Leveraging Technology for Better Outcomes
One of the key advantages of PEVAR is its minimally invasive nature, which can lead to reduced operating times, shorter hospital stays, and faster patient recovery. IT professionals can play a vital role in this process by ensuring that the necessary imaging and data management technologies are in place to support the PEVAR procedure.
For instance, the use of high-quality CT angiography, as seen in the Asian study cohort, is crucial for accurately assessing the CFA and monitoring changes over time. IT professionals can work closely with healthcare providers to implement robust imaging and data storage systems that enable seamless access to pre- and post-operative scans, facilitating comprehensive analysis and informed decision-making.
Fostering Collaboration and Knowledge Sharing
Another important aspect of optimizing PEVAR outcomes is the sharing of knowledge and best practices among healthcare professionals. IT professionals can play a pivotal role in facilitating this exchange of information, leveraging their expertise in data management and communication technologies.
By creating secure online platforms or collaborative networks, IT professionals can enable clinicians to share their experiences, discuss challenging cases, and collectively identify strategies for improving patient care. This collaborative approach can lead to the development of standardized protocols, the identification of emerging trends, and the rapid dissemination of innovative solutions.
Embracing Continuous Improvement
As the field of endovascular aneurysm repair continues to evolve, IT professionals must be proactive in staying up-to-date with the latest advancements and their implications for patient care. This may involve attending industry conferences, participating in online forums, or engaging in ongoing training and education programs.
By maintaining a deep understanding of the technological landscape and the clinical needs of PEVAR procedures, IT professionals can contribute to the continuous improvement of patient outcomes. This could include identifying opportunities for automation, streamlining data workflows, or implementing predictive analytics to anticipate and address potential complications.
Conclusion
The investigation into the anatomical effects of PEVAR on the CFA highlights the critical role that IT professionals can play in supporting the delivery of high-quality, patient-centric healthcare. By leveraging technology, fostering collaboration, and embracing continuous improvement, IT professionals can contribute to the ongoing optimization of percutaneous endovascular aneurysm repair and ensure that patients receive the best possible care.
As the IT Fix community continues to explore the intersection of technology and healthcare, I encourage you to stay informed, engage with clinicians, and explore innovative solutions that can transform the way we approach complex medical procedures like PEVAR. Together, we can drive progress, enhance patient outcomes, and contribute to the advancement of the IT industry.












