The Transformation of Medical Diagnostics
In the dynamic realm of healthcare, the field of digital pathology has emerged as a catalyst for a profound paradigm shift, revolutionizing the way medical professionals diagnose and manage diseases. This transformative approach has seamlessly integrated advanced technology, data analysis, and clinical expertise to redefine the landscape of patient care.
Pathology, a cornerstone of modern medicine, has long relied on the manual examination of tissue samples and cytological specimens to uncover invaluable insights into the identification and prognosis of various conditions. However, the traditional pathology framework, rooted in physical glass slides and localized expert consultations, has faced inherent limitations that have hindered efficiency, collaboration, and accessibility.
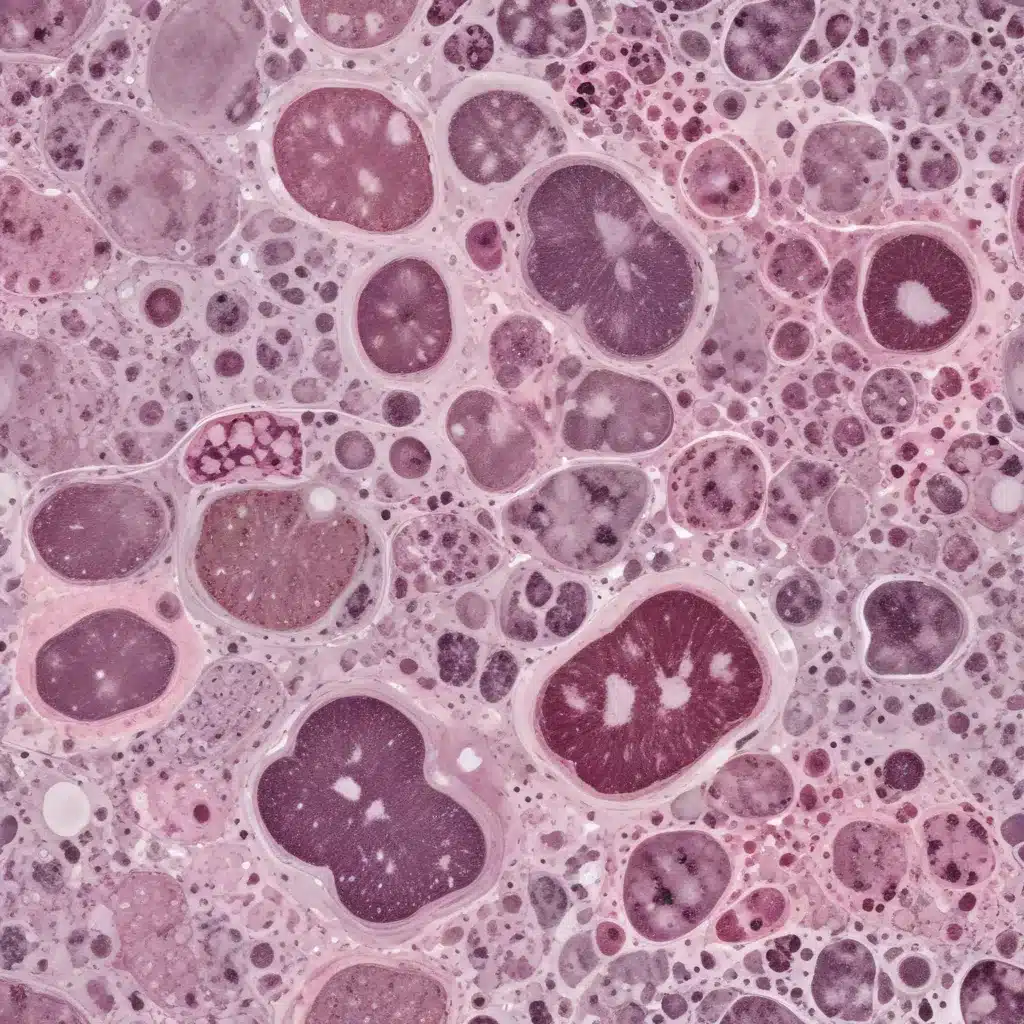
The advent of digital pathology has provided a solution to these constraints, ushering in a new era of medical diagnostics. This revolutionary approach involves the conversion of glass slides into high-resolution digital images, a process known as whole slide imaging (WSI). WSI has empowered pathologists with exceptional data storage, effortless sharing, and advanced analytical capabilities, transcending the boundaries imposed by physical slides.
The Fundamental Principles of Digital Pathology
At the heart of digital pathology lies the transformative power of WSI. This technology utilizes sophisticated scanners to capture comprehensive digital reproductions of entire glass slides, preserving the intricate cellular structures and subtle nuances observed under a conventional microscope. The resulting digital images can be navigated and examined at various magnifications, mirroring the experience of using a physical microscope.
Complementing WSI, the integration of image analysis techniques, particularly those driven by artificial intelligence (AI), has further enhanced the capabilities of digital pathology. AI algorithms can detect, measure, and classify cellular structures and abnormalities within the digital images, providing pathologists with valuable tools to improve the accuracy and efficiency of diagnostic processes.
Advantages of Digitizing Pathology Slides
The adoption of digital pathology has unlocked a myriad of benefits that have transformed various aspects of medical practice, including diagnostics, research, and education.
Efficient Storage and Retrieval: Digital pathology addresses the logistical challenges associated with the physical storage of glass slides, offering efficient electronic storage solutions. A single digital copy can replace numerous physical slides, reducing space requirements and facilitating effortless retrieval.
Seamless Sharing and Remote Consultations: Digital pathology has transcended geographical boundaries, enabling pathologists to share and analyze digitized slides remotely, regardless of their physical location. This feature has revolutionized the field of remote consultations, allowing experts worldwide to collaborate and provide their insights without the constraints of physical proximity.
Enhanced Access to Specialized Expertise: In areas with limited access to specialized medical resources, digital pathology has emerged as a crucial solution. The ability to remotely transmit digitized slides connects local practitioners with distant experts, facilitating accurate diagnoses and precise treatment recommendations.
Enriched Educational Opportunities: Digital pathology has transformed the learning environment for aspiring pathologists. Institutions can curate comprehensive digital repositories of pathological images, exposing students to a broader spectrum of medical conditions and enhancing their practical experience.
Quantitative Insights and Research Advancements: The integration of digital pathology, AI, and image analysis has opened up new frontiers in medical research. Scientists can investigate the associations between cellular characteristics and disease outcomes, potentially leading to the discovery of novel biomarkers, prognostic indicators, and therapeutic targets.
Remote Consultations and Telepathology: Enhancing Diagnostic Reach
The advancement of digital pathology has ushered in a groundbreaking method known as telepathology, which redefines the concept of remote consultations. By digitizing pathology slides, pathologists can now provide their expertise and insights to healthcare providers located anywhere in the world, overcoming the limitations of physical distance.
Remote Consultations Redefined by Digital Pathology
The core of telepathology revolves around the ability to enable remote consultations. The conventional barriers imposed by geographical separation are now eliminated, as pathologists can leverage the power of digitized slides to share their expertise and collaborate with peers across the globe.
Quantitative data highlights the growing adoption and perceived value of telepathology among healthcare professionals. According to a study published in the Journal of Pathology Informatics, a significant majority of surveyed pathologists, approximately 87%, expressed their belief that telepathology is a valuable tool for expert consultation. Furthermore, the findings indicate that approximately 71% of participants perceived telepathology as enhancing their diagnostic accuracy.
The Advantages of Telepathology in Enhancing Patient Care
The implementation of telepathology has far-reaching implications for patient care, particularly in underserved regions where access to specialized medical expertise is limited or geographically distant.
Enhanced Accessibility to Specialized Expertise: Telepathology serves as a vital tool in overcoming the geographical barriers that often impede the availability of specialized diagnostic insights. In areas with limited medical resources, this approach empowers local practitioners by facilitating their connection with experienced pathologists located in other regions, ensuring that patients receive the same standard of care as those in well-resourced areas.
Expedited Second Opinions: Telepathology demonstrates exceptional proficiency in facilitating prompt access to second opinions, a crucial component in complex cases. In situations where the initial diagnosis is uncertain, remote consultation allows for a thorough evaluation by specialists, decreasing the duration of patient uncertainty and simplifying the process of developing accurate treatment plans.
Promoting Collaboration Among Subspecialties: Instances that require specialized expertise often call for the collaboration of pathologists with distinct subspecialties. Telepathology serves as a means to facilitate this multidisciplinary approach, enabling experts from various fields to collectively examine cases and provide comprehensive insights, ultimately impacting treatment choices and improving patient outcomes.
Continuous Medical Education: Telepathology functions as a valuable educational tool, facilitating the exchange of knowledge and experiences among pathologists. Trainees have the opportunity to engage in the observation and acquisition of knowledge from experienced professionals, thereby fostering the cultivation of comprehensive expertise and the growth of their professional capabilities.
The Evolution of Patient-Centric Diagnostics
Telepathology, enabled by digital pathology, has transcended the limitations of conventional diagnostics, empowering pathologists to expand their expertise on a global scale. The data-driven insights confirm the growing acceptance and the advantages it provides to patient care.
Telepathology represents more than just a technological advancement; it serves as a transformative agent that effectively addresses disparities in healthcare accessibility, enhances diagnostic precision, and promotes collaborative expertise. In a time characterized by persistent healthcare inequalities, telepathology emerges as a promising solution, advocating for patient-centered diagnostics that transcend geographic limitations.
AI-assisted Analysis: Transforming Diagnostic Accuracy
The convergence of artificial intelligence (AI) and digital pathology has ushered in a transformative era, revolutionizing the field of medical diagnostics. This narrative delves into the mutually beneficial relationship between AI and digital pathology, exploring the potential of AI-assisted analysis to enhance diagnostic accuracy and efficiency.
The Profound Impact of AI in Digital Pathology
The fundamental aspect of this evolution is the capability of AI to analyze extensive datasets, detect complex patterns, and derive insights that surpass human perception. By leveraging AI’s computational capabilities, digital pathology has the potential to enhance the accuracy of diagnoses and optimize the process of making informed decisions.
Quantitative data showcases the growing recognition and adoption of AI tools among pathologists. A study published in the Journal of Pathology Informatics found that around 60% of pathologists currently utilize AI in their professional practice, and approximately 35% of pathologists intended to incorporate AI into their training in the foreseeable future.
Revealing the Applications of AI
The wide range of AI applications in digital pathology has transformed tasks that were once time-consuming and reliant on subjective judgment.
Image Recognition and Classification: The advanced capabilities of AI in image recognition have greatly enhanced its significance in the field of digital pathology. Algorithms possess the ability to analyze cellular structures and detect subtle variations that may indicate the presence of pathological conditions, expediting the assessment process and resulting in prompt detection and intervention.
Pattern Analysis for Anomalies: The ability of AI to recognize patterns enables advanced diagnostic analysis. Algorithms can detect anomalous features that may elude human observation, minimizing false negatives and enhancing the accuracy of diagnoses.
Predictive Modeling and Prognosis: The predictive modeling capabilities of AI offer significant potential in accurately predicting the progression of diseases. By analyzing large datasets, AI algorithms can identify correlations between cellular characteristics and patient outcomes, assisting in the development of personalized treatment strategies.
Utilization of Data-driven Insights: The capability of AI to analyze datasets and identify patterns dramatically enhances the process of making well-informed decisions. Algorithms can analyze patient histories and diagnostic data, assisting pathologists in determining the most effective treatment strategies.
The integration of AI into the field of digital pathology signifies a significant and transformative advancement in medical diagnostics. The available quantitative data confirms the increasing adoption of AI tools among pathologists, providing evidence of its potential to revolutionize diagnostic practices.
Challenges and Considerations
As healthcare institutions navigate the transition toward digital pathology, they face various challenges that require thoughtful consideration and effective solutions.
Data Security and Privacy Concerns
The digitization of pathology slides raises significant concerns regarding data security and patient information confidentiality. Ensuring the safety of digitized patient information from unauthorized access and breaches is paramount. Healthcare organizations must implement robust security measures to safeguard invaluable medical data.
Standardization and Interoperability
Achieving consistent standards and interoperability is crucial for the effective implementation of digital pathology. The absence of uniformity in labeling, formatting, and metadata can hinder effective collaboration and remote consultations. Addressing these challenges is essential for unlocking the full potential of digital pathology.
Regulatory Compliance
Compliance with rigorous regulations governing medical data and laboratory practices is a critical consideration. Adhering to regulations such as the Health Insurance Portability and Accountability Act (HIPAA) is essential to mitigate potential legal consequences and ensure the responsible use of digital pathology.
Pathologist Training and Skill Enhancement
Effective implementation of digital pathology requires a highly skilled workforce proficient in utilizing digital tools and interpreting insights generated by AI. Implementing structured training programs to equip pathologists with the necessary skills for precise diagnosis and streamlined workflow is essential.
The integration of AI in digital pathology presents an additional challenge, as pathologists must be able to critically evaluate the recommendations provided by AI systems and make well-informed clinical decisions. Striking the right balance between human expertise and AI augmentation is crucial to ensuring accurate diagnoses and maintaining the pathologist’s role as the ultimate decision-maker.
As the healthcare industry continues to embrace the transformative potential of digital pathology, addressing these challenges is paramount. By prioritizing data security, establishing comprehensive standards, ensuring regulatory compliance, and providing robust training, institutions can effectively leverage the revolutionary capabilities of digital pathology while maintaining the utmost commitment to patient care and safety.
Case Studies and Examples: Demonstrating the Impact of Digital Pathology
The integration of digital pathology and AI has profoundly impacted the healthcare industry, leading to advancements in diagnostics and patient care. Concrete examples from leading healthcare institutions and research centers serve as tangible demonstrations of the considerable impact of this technological revolution.
The Montefiore: Enhancing Diagnostic Capabilities through AI-powered Insights
The Montefiore, a renowned institution known for its dedication to pioneering advancements, has partnered with Paige.AI to implement an AI-powered platform that aids pathologists in the diagnosis of prostate cancer. The platform has been trained using a comprehensive collection of pathology slides and aims to enhance pathologists’ expertise by identifying and highlighting areas of interest and potential abnormalities.
The effectiveness of this AI-assisted system was demonstrated in a study published in JAMA Oncology. The pathologists utilizing the platform showed superior performance compared to their traditional counterparts, achieving an accuracy rate of 86% as opposed to 70%. The AI tool accelerated the diagnostic process and showcased its potential to improve accuracy, establishing a basis for more efficient treatment decisions.
Royal Philips and Amsterdam University Medical Centers (UMC): Redefining Oncology Diagnostics
Royal Philips and Amsterdam University Medical Centers (UMC) have initiated a collaborative effort to redefine oncology diagnostics by leveraging digital pathology. The partnership resulted in the development of an AI-powered platform that demonstrates exceptional accuracy in identifying breast cancer metastases in lymph nodes. The platform incorporates sophisticated image analysis algorithms, allowing pathologists to detect subtle cellular characteristics that may indicate the presence of malignancy.
A study conducted by the partnership has yielded significant and groundbreaking findings. The AI-powered platform has achieved a sensitivity rate of 89.4%, which exceeds the accuracy rate of traditional pathologists (74.5%) in identifying breast cancer metastases. This demonstrates the practical value of AI in improving diagnostic capabilities, especially in intricate cases that demand careful examination.
Massachusetts General Hospital (MGH): Predicting Genetic Mutations in Brain Tumors
Massachusetts General Hospital (MGH) has undertaken an innovative initiative to utilize digital pathology and AI to improve neurosurgical decision-making. In partnership with Path AI, MGH has successfully developed an advanced AI model that accurately predicts genetic mutations within brain tumors.
The predictive capability of this tool assists healthcare professionals in customizing treatment approaches according to the unique profiles of individual patients. The success of the AI model was highlighted in a research publication in Nature Medicine, emphasizing its quantitative impact. The model exhibited a precision rate of 94.6% in its ability to predict genetic mutations in brain tumors, providing neurosurgeons with valuable insights essential for developing personalized treatment plans and ultimately improving patient outcomes.
These case studies provide valuable insights into the significant effects of incorporating digital pathology and AI into healthcare workflows. The available quantitative data provides strong evidence supporting the effectiveness of AI in enhancing diagnostic accuracy, optimizing processes, and ultimately enhancing the quality of patient care.
Future Directions: Exploring the Progression of Digital Pathology
As the medical technology landscape continues to evolve, the trajectory of digital pathology showcases a compelling narrative of progress. The potential future advancements in this field have the capacity to significantly reshape diagnostics, research, and healthcare management at a global level.
Advancements in AI and Automation: A Preview of the Future
The convergence of digital pathology and AI presents significant potential, with the capacity to revolutionize the diagnostic field in unprecedented ways. The future foresees the advancement of AI algorithms into highly sophisticated systems that aid in anomaly detection and forecast disease trajectories. With the accumulation of more data, it is expected that machine learning models will experience a significant increase in their predictive accuracy, providing clinicians with valuable insights into disease progression and potential outcomes.
Integration with Electronic Health Records (EHRs): The Convergence of Data
Integrating digital pathology with EHRs represents a notable advancement in delivering comprehensive patient care. By effectively incorporating pathology data with a patient’s medical history, clinicians can gain a comprehensive understanding of their condition. The future presents the potential for interoperable systems that enable seamless real-time data exchange, empowering healthcare providers with comprehensive insights into each patient’s health journey.
Advancing Research and Enhancing Population Health Management
The potential of digital pathology as a catalyst for groundbreaking research endeavors is promising in the future. The integration of extensive datasets derived from digital pathology slides, EHRs, and genetic information has the potential to drive revolutionary advancements in research and discovery. AI-powered analyses can reveal concealed correlations, detect previously unknown biomarkers, and offer valuable insights into the causes of diseases, thereby guiding research efforts toward more precise interventions.
Ethical and Legal Considerations: Navigating the Complexities
As the landscape of digital pathology evolves, ethical and legal considerations come into play to ensure compliance and accountability. Patient data privacy, informed consent, responsible AI use, regulatory approvals, and liability concerns form the ethical and legal scaffolding upon which this paradigm rests.
Healthcare institutions must prioritize the protection of patient confidentiality, ensuring robust data security measures and transparent communication regarding the use of digital pathology and AI-driven insights. Regulatory bodies, such as the Food and Drug Administration (FDA), play a crucial role in validating the safety and effectiveness of digital pathology solutions, upholding the commitment to patient safety and clinical reliability.
The convergence of human expertise and AI-driven insights introduces complexities in determining accountability, highlighting the need for a harmonious collaboration between healthcare professionals and technology experts. Navigating these ethical and legal considerations is essential to ensure the responsible and pioneering progress of digital pathology.
Conclusion: Embracing the Promise of Digital Pathology
The ongoing trajectory of digital pathology showcases a transformative landscape, where technology and medical expertise converge to redefine the future of healthcare diagnostics. By seamlessly integrating advanced imaging, data analysis, and collaborative networks, digital pathology has transcended the limitations of conventional pathology practices, offering a glimpse into a future marked by enhanced accessibility, precision, and personalized care.
As the field continues to evolve, the promise of digital pathology lies in its ability to empower healthcare providers, emancipate patients, and drive groundbreaking research. Through the synergistic collaboration of human expertise and technological innovation, the healthcare community is poised to address pressing medical challenges with unparalleled effectiveness, ultimately improving patient outcomes and transforming the very fabric of modern medicine.
The journey ahead may present complexities, but the unwavering commitment to ethical responsibility and legal prudence will guide the pioneers of digital pathology toward a future where innovation and compassion converge, ushering in a new era of patient-centric diagnostics and personalized healthcare solutions.












