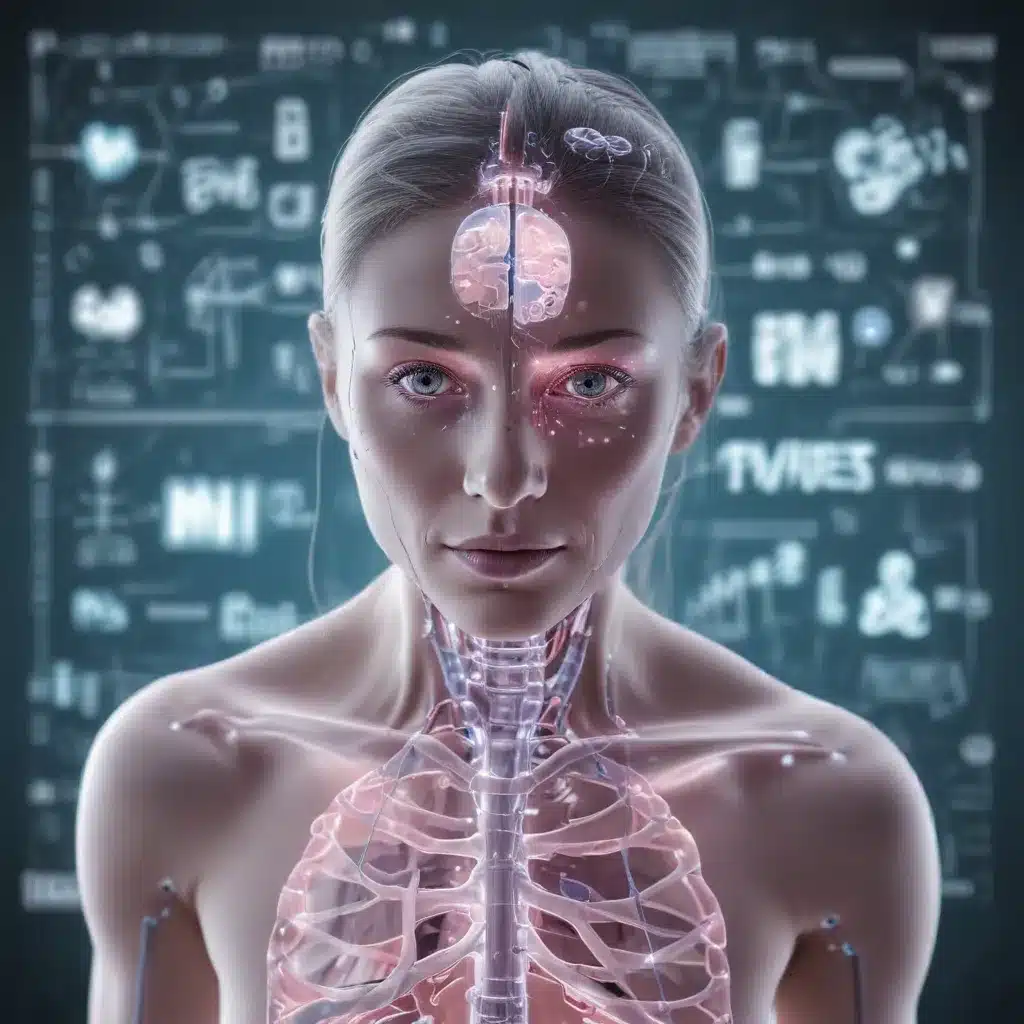
The Convergence of AI and Precision Medicine
The convergence of artificial intelligence (AI) and precision medicine promises to revolutionize healthcare. Precision medicine aims to personalize care for every individual, requiring access to massive amounts of data, such as data collected through initiatives like the UK Biobank and the All of Us project. This goal is enabled by the rapid digitization of health-related data and the increasing adoption of technology in the industry.
AI leverages sophisticated computation and inference to generate insights, empowering clinicians through “augmented intelligence.” Recent literature suggests that translational research exploring the convergence of AI and precision medicine will help solve the most difficult challenges facing personalized care, especially those involving non-genomic and genomic determinants combined with patient symptoms, clinical history, and lifestyle factors.
Three main principles for successful AI adoption in healthcare include:
- Data and Security: Ensuring full transparency and trust in how AI systems are trained and the data/knowledge used to train them.
- Analytics and Insights: Providing “augmented intelligence” and “actionable insights” that support what humans do, not replace them.
- Shared Expertise: Recognizing the complementary relationship between AI systems and human professionals, leading to necessary workforce changes and new skills.
The Power of AI in Healthcare
AI technologies in medicine exist in many forms, from the purely virtual (e.g., deep-learning-based health information management systems) to cyber-physical (e.g., robots assisting surgeons). The power of AI to recognize sophisticated patterns and hidden structures has enabled many image-based detection and diagnostic systems to perform as well as or better than clinicians.
AI-enabled clinical decision-support systems can reduce diagnostic errors, augment intelligence to support decision-making, and assist clinicians with EHR data extraction and documentation tasks. Advances in natural language processing (NLP), pattern identification, efficient search, prediction, and bias-free reasoning will lead to further AI capabilities in addressing currently intractable problems.
The Evolution of Precision Medicine
Precision medicine is perhaps best described as a healthcare movement involving the development of a “New Taxonomy of human disease based on molecular biology.” The field has evolved to recognize how the intersection of multi-omic data combined with medical history, social/behavioral determinants, and environmental knowledge precisely characterizes health states, disease states, and therapeutic options for affected individuals.
Precision medicine offers healthcare providers the ability to discover and present information that either validates or alters the trajectory of a medical decision from one based on evidence for the average patient to one based on an individual’s unique characteristics. Advances in precision medicine manifest into tangible benefits, such as early detection of disease and designing personalized treatments.
The Convergence of AI and Precision Medicine
The convergence of AI and precision medicine is transforming healthcare in several ways:
-
Genome-Informed Prescribing: AI techniques have proven useful for efficient and high-throughput genome interpretation, enabling personalized medications and dosages.
-
Radiogenomics: AI is establishing associations between cancer imaging features and gene expression to predict a patient’s risk of developing toxicity following radiotherapy.
-
Predicting Treatment Response: AI demonstrates potential applications in using gene expression data to predict patient response to chemotherapy.
-
Incorporating Environmental Considerations: AI has provided numerous examples of augmenting diagnostic capabilities in resource-poor locations, which may translate into better patient classification and more personalized therapy planning.
-
Clinical Factor Analysis: AI has emerged as a central pillar in stratifying patients for therapy based on factors like age, co-morbidities, and organ function.
Personalized Prevention and Risk Prediction
The broad availability of genetic information offered by next-generation sequencing and direct-to-consumer testing has made personalized prevention and management of serious diseases a reality. AI approaches that excel at discovering complex relationships among a large number of factors provide opportunities for early disease detection and risk prediction.
AI-enabled recognition of phenotype features through EHRs or images and matching those features with genetic variants may allow faster genetic disease diagnosis. Automated speech analytics have also benefited from improvements in NLP, providing indicators for early assessment and detection of conditions like dementia, Parkinson’s, and mental disorders.
AI-Powered Diagnostics and Monitoring
AI-based image analysis aimed at improving disease risk prediction and diagnosis is increasingly being used for detecting diabetic retinopathy, metastasis in cancer, and benign melanoma. The widespread use of home monitoring and wearable devices has fueled new, noninvasive, wearable applications for monitoring and detecting specific health conditions.
Digital biomarkers are expected to facilitate remote disease monitoring outside of the hospital setting and support decentralized clinical trials. Wearable tools that provide continuous multidimensional measurements of preselected biomarkers would enable the detection of minimum residual disease and monitor disease progression.
Challenges and Considerations
While the use of AI in precision medicine has shown promising experimental results, successful transformation into real-world applications depends on factors beyond just accuracy, such as reliability, safety, and generalizability.
Key challenges include:
-
Fairness and Bias: Addressing biases in the data and models used to train AI systems to ensure equitable and unbiased decision-making.
-
Socio-Environmental Factors: Validating AI models in the clinical environment and considering the impact of various conditions and workflows on model performance.
-
Data Safety and Privacy: Building a safe and well-controlled ecosystem for data storage, management, and sharing, and addressing regulatory and privacy concerns.
Addressing these challenges through collaborative efforts between the AI and biomedical communities, as well as developing innovative data annotation methods and rigorous AI techniques, will be crucial for the responsible and effective implementation of AI in healthcare.
The Future of AI in Healthcare
As AI and precision medicine continue to converge, the future of healthcare holds immense promise. Predictive analytics, personalized medicine, and AI-powered diagnostics and monitoring will revolutionize patient care, enabling earlier disease detection, more targeted treatments, and improved health outcomes.
While challenges around data quality, privacy, and ethical considerations must be addressed, the integration of AI in healthcare is expected to transform the industry, leading to enhanced efficiency, reduced costs, and better access to personalized care. By harnessing the full potential of AI, healthcare organizations can improve patient experiences, empower clinicians, and ultimately, revolutionize the way medicine is practiced.
The convergence of AI and precision medicine is a testament to the transformative power of technology in healthcare. As we continue to push the boundaries of what is possible, the future of healthcare looks brighter than ever, with AI-driven innovations poised to improve the lives of patients and healthcare professionals alike.












